Stages of Gum Disease
Gingivitis vs. Periodontitis
Gingivitis is the earliest stage of gum disease, which is often reversible with proper oral hygiene. Periodontitis, however, is an advanced stage that can cause irreversible damage to the gums and bone structure. Understanding the difference helps patients realize the urgency of treating gum disease early.
Complications Linked to Untreated Gum Disease
If gum disease is left untreated, it can lead to a range of severe complications:
- Tooth Loss: As gum disease progresses, it weakens the support structures of your teeth, eventually leading to tooth mobility and possible loss.
- Gum Recession: The gums may begin to pull away from the teeth, exposing the roots and making teeth more susceptible to decay and sensitivity.
- Bone Loss: Advanced gum disease can cause the bone supporting your teeth to deteriorate, which can lead to the need for costly surgeries like bone grafts or tooth extractions.
- Abscesses: Untreated infections can result in painful abscesses, which are pockets of pus that form in the gums. These abscesses may require surgical drainage and further treatments.
Connection to Overall Health Issues
Gum disease is not just a local issue—it has been linked to several serious systemic conditions. Here’s how it can impact your overall health:
- Heart Disease: Gum disease has been shown to increase the risk of heart disease. Infected gums may allow bacteria to enter the bloodstream, leading to inflammation that can affect the heart.
- Stroke: The inflammation caused by gum disease can also increase the risk of a stroke, as it may contribute to the formation of blood clots.
- Diabetes: People with diabetes are more likely to develop gum disease, and untreated gum disease can also make it harder to control blood sugar levels. The inflammation from gum disease can worsen the body’s response to insulin.
- Respiratory Infections: The bacteria from gum disease can travel to the lungs, increasing the risk of respiratory infections like pneumonia.
By treating gum disease early, you can help prevent not only oral health issues but also reduce your risk of developing these serious conditions. This underscores the broader implications of untreated gum disease, making early intervention even more important for your overall health.
Diagnosis and Evaluation
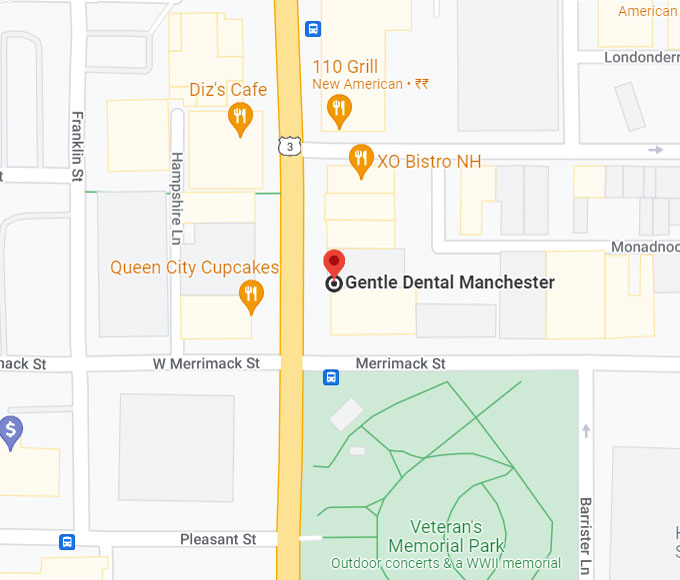
Accurate diagnosis is the first step in effectively treating gum disease. At Gentle Dental, we prioritize a thorough evaluation to understand the severity of the condition, and we reassure patients that the process is gentle and minimally uncomfortable.
How Dentists Diagnose Gum Disease
When you visit Gentle Dental, your dentist or hygienist will perform a comprehensive exam to assess your gum health. This exam includes:
- Gum Pocket Measurement: The dentist will measure the depth of the pockets around your teeth using a specialized tool. Healthy gums usually have shallow pockets, but deeper pockets can indicate gum disease.
- Gum Recession and Infection Check: The dentist will look for signs of gum recession (where the gums pull away from the teeth) and check for infections that could be causing swelling, bleeding, or pain in your gums.
- Evaluation of Tooth Mobility: In advanced cases, the dentist may check if any teeth are loose or moving due to damage to the bone structure caused by gum disease.
- X-rays: X-rays may be used to check for bone loss that often occurs in severe gum disease cases. These images help your dentist evaluate the health of the bone supporting your teeth.
Tests and Tools Used in Diagnosis
Periodontal Probing:
This tool is used to measure the depth of gum pockets around your teeth. If the pockets are deeper than 3 millimeters, it indicates that the gums are pulling away from the teeth, which is a sign of gum disease. The dentist will gently insert the probe into these pockets to assess the extent of the disease.
X-rays:
X-rays are an essential tool to detect bone loss that is not visible to the naked eye. When gum disease is left untreated, it can cause the bones that support your teeth to deteriorate. X-rays help identify this early, enabling more effective treatment to prevent further damage.
Treatment Approaches
Gum disease treatment can vary depending on the severity of the condition. Early-stage gum disease (gingivitis) typically requires non-surgical treatments, while more advanced cases (periodontitis) may require surgical procedures. Below is a breakdown of available treatment options for gum disease:
Non-Surgical Treatments
1. Scaling and Root Planing
What it is: This is a deep cleaning procedure that removes plaque and tartar from below the gumline. It’s often the first line of defense in treating gum disease.
How it works: The dentist or hygienist uses specialized tools to clean the surfaces of your teeth and under your gums. Root planing smooths the root surfaces of your teeth to help gums reattach and reduce the likelihood of bacteria buildup.
When it’s used: Scaling and root planing is usually recommended for mild to moderate gum disease (gingivitis or early periodontitis).
2. Antibiotic Therapy
What it is: Antibiotics are used to treat bacterial infections in the gums and prevent the infection from spreading.
How it works: Antibiotics can be prescribed in pill form or applied directly to the affected areas in the form of gels, rinses, or even slow-release devices placed in the gum pockets.
When it’s used: Antibiotics are often used alongside scaling and root planing to help control bacteria and reduce inflammation in early to moderate gum disease.
Surgical Treatments
If gum disease progresses to periodontitis and non-surgical treatments are insufficient, surgical procedures may be necessary to repair damage and restore gum health.
- Pocket Reduction Surgery: This procedure reshapes the gums to reduce deep pockets that form around the teeth.
- Bone and Gum Grafting: Bone and gum grafting are restorative procedures used to repair damaged bone and gum tissue that has been lost due to periodontal disease.
- LANAP (Laser-Assisted New Attachment Procedure): A minimally invasive laser treatment for gum disease that eliminates the need for cutting or stitching.
Additional Treatment Options
- Laser Therapy (Non-LANAP): Laser therapy uses focused light to remove infected tissue from the gum pockets. It can be used as an alternative to scalpel-based procedures.
- Arestin®: Arestin® is a localized antibiotic treatment that is applied directly into the gum pockets after scaling and root planing.
Prognosis and Recovery
What to Expect After Treatment:
- Non-Surgical Treatments (Scaling and Root Planing): Mild swelling and discomfort for a few days. Pain can be managed with over-the-counter pain relievers. A soft diet and gentle oral care are recommended.
- Surgical Treatments (e.g., Pocket Reduction Surgery, Gum Grafting): Longer recovery time with significant swelling and bruising. Discomfort may require prescription pain management. Avoid certain foods and follow aftercare instructions carefully.
Long-term Management of Gum Health:
- Regular follow-up visits to monitor healing and gum health.
- Increased frequency of cleanings, especially during the first year after treatment.
- At-home oral hygiene must be maintained with regular brushing and flossing.
- Professional cleanings remove plaque and tartar buildup, preventing recurrence.
Preventive Measures
How to Prevent Gum Disease:
- Daily Oral Hygiene: Brush your teeth at least twice a day with fluoride toothpaste. Floss once a day to clean between teeth and along the gumline.
- Antimicrobial Mouthwash: Use to kill bacteria and reduce gum inflammation.
- Regular Dental Check-ups: Visit your dentist regularly for professional cleanings and early detection of gum disease. Professional cleanings help remove tartar (hardened plaque), which cannot be removed by brushing alone.
- Lifestyle Changes: Avoid smoking, as it increases the risk of gum disease and hampers healing. Eat a balanced diet with fruits, vegetables, and whole grains to support gum health.